Frontal fibrosing alopecia destroys hair follicles permanently. This scarring form of hair loss primarily affects women over 50, creating a distinctive band-like recession along the hairline. Unlike temporary thinning conditions, FFA involves immune-mediated inflammation that leaves a smooth, shiny scalp where follicles once thrived. Eyebrow loss frequently precedes scalp changes. Recognition of risk factors allows earlier intervention, potentially preserving remaining follicles before scarring becomes irreversible.
Key Takeaways
- FFA permanently destroys follicles through immune-mediated scarring. Once lost, they cannot regenerate.
- Postmenopausal women face the highest risk, though younger women and men can develop the condition.
- Hormonal exposures (HRT, pregnancy, thyroid dysfunction) and daily skincare products show statistical associations.
- Disease progresses through stages, so early intervention during active inflammation preserves remaining follicles.
- Medical treatments aim for stabilisation, not regrowth; most require 6-18 months to assess effectiveness.
- Scalp micropigmentation achieves 100% favourable outcomes in FFA patients due to mild atrophy.
- Psychological impact often exceeds physical changes; professional support helps navigate emotional challenges.
What Is Frontal Fibrosing Alopecia?
Frontal fibrosing alopecia represents a primary cicatricial (scarring) alopecia characterised by progressive hairline recession. First identified in 1994, this condition belongs to the lichen planopilaris family, sharing inflammatory patterns that permanently destroy hair follicles.
| Primary Symptoms | Secondary Signs |
| Symmetrical frontal hairline recession | Perifollicular redness during active phases |
| Eyebrow thinning or complete loss (80-90% of cases) | Facial papules near the hairline |
| Smooth, pale scalp texture in affected areas | Prominent forehead veins |
| Isolated “lonely hairs” persisting in bald patches | Occasional itching or burning sensations |
FFA differs from androgenetic alopecia through its scarring nature. Once follicles are destroyed, they cannot regenerate. The affected scalp appears shiny and lacks visible follicle openings.
What Causes Frontal Fibrosing Alopecia?

The precise cause remains unknown, though an autoimmune mechanism appears responsible. Your immune system mistakenly identifies hair follicles as foreign invaders, triggering T-lymphocyte attacks that create inflammation around follicle structures.
Contributing factors include:
- Immune dysregulation – CD8+ cytotoxic T cells infiltrate scalp tissue, generating chronic inflammation that destroys follicle stem cells.
- Genetic susceptibility – Identical twins developing FFA simultaneously, and genome-wide studies identifying four specific genetic loci suggest inherited vulnerability.
- Hormonal changes – Postmenopausal status dominance indicates reduced oestrogen, combined with androgen sensitivity, may activate dormant genetic predispositions.
- Environmental triggers – Unknown exposures potentially initiating the immune cascade in susceptible individuals.
FFA likely requires multiple factors converging. Some individuals carry genetic risk without developing symptoms until specific triggers activate the immune cascade.
Which Hormonal Changes Increase Your Risk of FFA?
Specific hormonal exposures significantly elevate FFA risk beyond natural menopause.
| Exposure | Increased Risk | Key Details |
| Hormone Replacement Therapy | 1.76 times | Whether oestrogen, progesterone, or treatment duration influences susceptibility remains unclear |
| Pregnancy History | 1.6 times | Multiple pregnancies may compound this effect |
| Raloxifene Use | Very high | No control patients exposed in studies, suggesting a particularly elevated risk |
| Hypothyroidism | 1.73 times | Thyroid hormones directly regulate follicle cycling and immune function |
| Hysterectomy with Oophorectomy | Variable | Abrupt ovarian hormone loss may trigger immune dysregulation |
These risk factors don’t guarantee FFA development, but they increase the probability in those already carrying genetic vulnerability. Untreated or poorly managed thyroid disease may create conditions favouring autoimmune follicle attacks.
Could Your Daily Products Be Triggering FFA Progression?

Evidence increasingly implicates everyday skincare products as potential triggers in genetically susceptible individuals.
Facial Sunscreen and Cosmetic Associations
Leave-on facial sunscreens show a striking correlation. Women face 1.6 times higher risk, and men show 11.6 times increased odds. Researchers discovered titanium nanoparticles embedded within the hair shafts of FFA patients. Some dermatologists report hairline improvement following sunscreen cessation, though other research finds no significant progression difference between users and non-users.
Anti-ageing creams (1.84 times risk), ordinary facial soaps (2.09 times), facial moisturisers (1.99 times), and formalin-containing hair straightening treatments (3.18 times) all show statistical associations.
Occupational Exposures
Workplace contact with alkylphenolic compounds, industrial chemicals in detergents, pesticides, and plastics, increases risk by 1.48 times. These endocrine-disrupting substances may interfere with hormonal signalling pathways.
The Balance
Establishing causation proves difficult. Whether products trigger initial immune activation or worsen pre-existing inflammation remains uncertain. The recommendation balance is really tricky. Discontinuing sun protection raises skin cancer risk, yet continuing suspect products might accelerate follicle destruction. Individual risk assessment with a specialist helps navigate these competing concerns.
What Other Conditions Increase Frontal Fibrosing Alopecia Risk?
Several medical conditions cluster with FFA, suggesting shared immune pathways or genetic vulnerabilities.
Autoimmune Disease Connections
Rosacea increases odds by 1.91 times, whilst lichen planus pigmentosus shows the strongest association, 5.14 times higher risk, and frequently precedes scalp hair loss. Patients with lupus erythematosus or rheumatoid arthritis face an elevated risk, suggesting broader immune dysregulation extending to hair follicles.
Genetic Evidence
Identical twin pairs developing FFA simultaneously provide compelling evidence. Beyond twins, first-degree relatives show increased incidence. No single gene causes FFA, multiple genetic variants likely contribute small individual effects that compound susceptibility.
Ethnic Variations
Women of African descent typically develop symptoms earlier (early 40s), with less obvious inflammation and frequent traction alopecia coexistence. Lichen planus pigmentosus commonly precedes hairline recession. Japanese women demonstrate less severe forms compared to European populations. These patterns indicate FFA is expressed differently across genetic backgrounds.
How Does Frontal Fibrosing Alopecia Progress Over Time?
Frontal Fibrosing Alopecia advances through distinct phases at unpredictable rates. Some patients experience rapid recession within months, whilst others see minimal changes over years.
Early Detection Window
Initial changes prove subtle. Slight hairline recession mimicking normal ageing. Perifollicular inflammation creates small bumps around individual hairs at the advancing edge. Redness and fine scaling appear during active phases. This early window offers the best intervention opportunity.
Active Progression Phase
Hairline recession averages 0.5-1 centimetre annually during active disease. Total recession typically measures 1.8-2.6 centimetres before stabilisation. Eyebrow loss intensifies, facial papules may emerge, and forehead veins become more prominent. A negative hair pull test indicates inflammation has subsided.
Advanced Scarring Stage
Complete follicle destruction leaves a smooth, shiny scalp devoid of follicular openings. Pigmentation changes create visible contrast between affected and unaffected areas. Biological regrowth becomes impossible without regenerative interventions still in research phases.
For those facing established scarring, scalp micropigmentation for alopecia offers cosmetic restoration by creating the appearance of hair follicles through specialised pigmentation techniques.
Why Is Early Stage Frontal Fibrosing Alopecia Treatment Critical?
FFA treatment on early stages preserves what remains rather than restoring what’s lost. This distinction shapes every clinical decision.
Scarred follicles cannot regenerate through current medical interventions. Once the inflammatory process destroys stem cells in the follicle bulge, that follicle’s hair-producing capacity ends permanently. Treatment during active inflammation can halt the immune attack, preventing additional follicles from entering the destruction pathway.
Dermoscopy reveals subtle changes invisible to the naked eye: absent follicular openings, white dots indicating scarring, and perifollicular scaling. A scalp biopsy provides a definitive diagnosis through histopathological examination showing lymphocytic infiltration patterns.
Atypical presentations delay recognition. Diffuse patterns, zig-zag recession, or isolated eyebrow loss without obvious hairline changes may postpone diagnosis by months or years. Average diagnostic delay following symptom onset ranges from six months to two years. Each month of untreated inflammation translates to additional follicle loss. By the time a smooth, shiny scalp develops, intervention can only prevent further progression. Existing damage becomes permanent.
What Medical Treatments Can Slow FFA Progression?

No cure exists, but existing FFA treatment aims at stabilisation—halting further recession whilst preserving remaining follicles. Medical evaluation remains necessary before starting any therapy.
FDA-Approved Treatment
Intralesional triamcinolone acetonide injections represent the only FDA-approved FFA treatment. Approximately 60% of patients experience improvement, with 80% achieving eyebrow regrowth when treated early. Risk involves worsening scalp atrophy with repeated injections.
Commonly Prescribed Medications
- 5-alpha-reductase inhibitors (finasteride, dutasteride) – particularly beneficial when androgenetic alopecia coexists.
- Hydroxychloroquine – may achieve remission; requires a 4-6 month trial and annual eye examinations.
- Tetracycline antibiotics (doxycycline, minocycline) – reduce inflammation through non-antibiotic mechanisms.
- Topical corticosteroids – limited effectiveness alone.
- Topical tacrolimus – suppresses immune activity at application sites.
- Immunomodulators (mycophenolate mofetil, ciclosporin) – dampen systemic immune responses.
- Low-dose oral minoxidil – emerging option showing promise.
- JAK inhibitors (tofacitinib, baricitinib) – novel approaches under investigation.
Most patients require 6-18 months before assessing treatment effectiveness. Success means stabilisation, not regrowth.
What Daily Changes Might Help Manage FFA?
Lifestyle modifications carry uncertain evidence but may reduce disease activity in some patients. Clinical observations suggest potential benefits, though no definitive studies prove specific changes halt progression.
Commonly recommended modifications:
- Sun protection – Switch from chemical sunscreens to wide-brimmed hats and UV-protective clothing.
- Facial products – Choose fragrance-free, mineral-free formulations; use dermatologist-recommended cleansers instead of ordinary soaps.
- Hair care – Avoid tight hairstyles, chemical straightening treatments, and excessive heat styling.
- Underlying conditions – Optimise thyroid medication dosing and manage coexisting autoimmune diseases.
- Scalp handling – Minimise mechanical trauma through gentle brushing and washing.
- Monitoring – Attend regular dermatologist appointments with standardised photography every six months.
These changes require balancing potential benefits against quality of life. Abandoning all suspected products creates anxiety that may outweigh uncertain gains. Selective, evidence-informed modifications prove more sustainable than wholesale lifestyle overhauls. Individual risk assessment with a specialist helps determine which adjustments make sense for your specific situation.
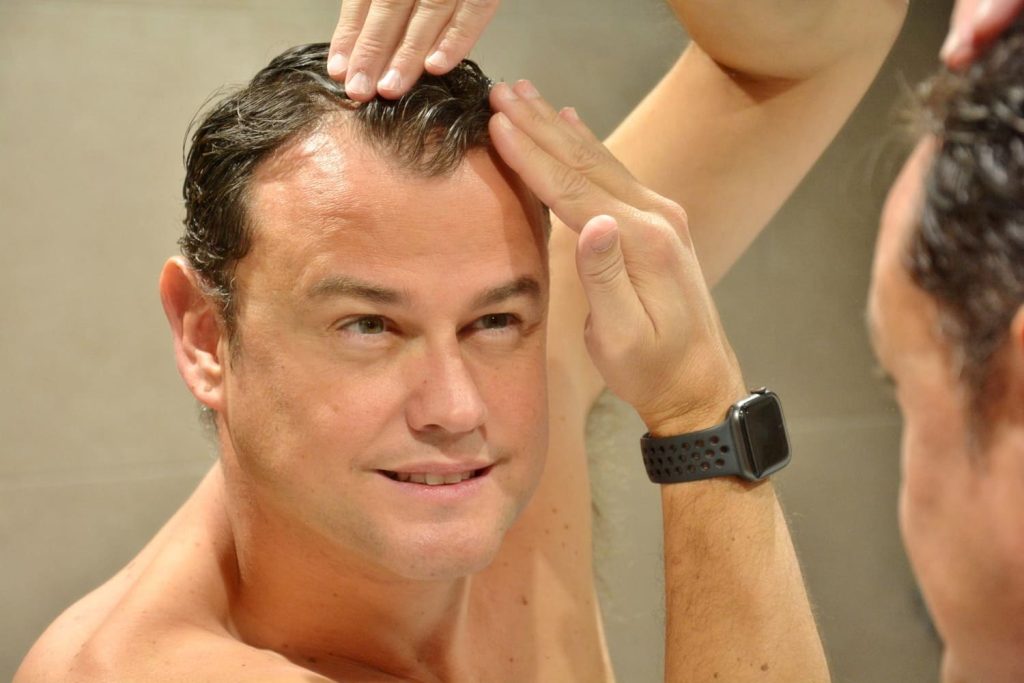
How Can You Camouflage FFA When Follicles Are Already Lost?
Cosmetic solutions restore appearance when permanent scarring prevents biological regrowth.
Scalp Micropigmentation Effectiveness
SMP for alopecia demonstrates particularly strong outcomes in FFA patients. Recent clinical studies report 100% favourable results, significantly higher than other scarring alopecias like morphea (20%) or lichen planopilaris (33.3%). FFA’s relatively mild atrophy allows superior pigment retention.
This hair tattoo solution creates the illusion of closely cropped hair through thousands of precisely placed pigment dots. Specialised needles deposit pigment at shallow depths (0.5-1.2mm), mimicking individual follicles. The technique proves effective across all skin tones with proper pigment matching.
Three to four sessions achieve optimal density, spaced 10-20 days apart. Results last 3-5 years before requiring touch-ups. The procedure works equally well for eyebrow restoration.
Alternative Options
- Custom hairpieces – Medical-grade wigs remain removable for ongoing treatments.
- Keratin fibres – Temporary daily application creates a density illusion.
- Microblading – Semi-permanent eyebrow tattooing lasting 12-18 months.
- Hair transplantation – Limited success due to scarring; high rejection rates.
Cosmetic interventions provide immediate confidence restoration whilst medical management continues. Many patients combine approaches, medications preventing further loss, whilst micropigmentation addresses existing damage.
How Do You Cope With the Emotional Impact of FFA?
Hair loss alters how you perceive yourself and navigate the world. The psychological weight often exceeds physical changes, affecting professional confidence, social comfort, and intimate relationships. Younger patients typically experience heightened distress. Social situations that once felt natural become sources of anxiety.
Professional guidance:
- Dermatologists managing medical aspects
- Trichologists specialising in hair and scalp health
- Therapists addressing body image concerns
- Cosmetic practitioners offering camouflage solutions
Community connections through support groups provide an invaluable perspective from others navigating similar experiences. Grief over appearance changes deserves acknowledgement rather than dismissal. Your path toward emotional equilibrium remains deeply personal. Cosmetic solutions often restore confidence more rapidly than medical interventions.
Moving Forward With FFA
Risk factors reveal who faces a higher likelihood, though genetic susceptibility remains unchangeable. Medical interventions perform best during active inflammation, whilst cosmetic solutions restore appearance after scarring occurs. Professional dermatological care combined with realistic expectations provides the best path through both physical changes and emotional challenges. Hairline recession or eyebrow thinning warrants specialist assessment—earlier consultation preserves more options and potentially more follicles.
For personalised assessment of your hairline concerns or to explore cosmetic restoration options, book a free consultation with our qualified trichologist and scalp micropigmentation specialists.
FAQ
Can frontal fibrosing alopecia be reversed once hair follicles are scarred?
No, scarred follicles cannot regenerate naturally with current treatments. Medical interventions slow or halt progression, but don't restore already-destroyed follicles.
Should I stop using sunscreen if I'm concerned about FFA?
Dermatologists generally advise against stopping sun protection due to skin cancer risks. Consider switching to mineral-free formulations or using physical barriers like hats instead.
How long does it take to see if treatments are working for FFA?
Most medical treatments require 6-18 months of consistent use before assessing effectiveness. Success is measured by stabilisation (no further progression) rather than regrowth.
Can men develop frontal fibrosing alopecia?
Yes, though it's much rarer in men and typically involves stronger genetic factors. Men may present differently, sometimes with sideburn loss as the only initial feature.
Is there a blood test to diagnose FFA?
No specific blood test diagnoses FFA, though thyroid function tests may identify associated conditions. Diagnosis relies on clinical examination, dermoscopy, and scalp biopsy.
Can FFA affect hair on other parts of the body besides the scalp?
Yes, FFA can cause loss of eyelashes, sideburns, facial hair, and body hair on arms, legs, underarms, and pubic areas. Extensive body hair involvement suggests more severe disease.




No comment yet, add your voice below!